Palliative Medicine is a specialized field focused on improving the quality of life for patients with serious, chronic, or life-limiting illnesses. It addresses not only physical symptoms but also emotional, social, and spiritual needs. It prevents and relieves suffering through the early identification, correct assessment and treatment of pain and other problems, whether physical, psychosocial or spiritual. (https://www.who.int/news-room/fact-sheets/detail/palliative-care)
What is a typical day as a Palliative Medicine Specialist?
– Assessing hospitalized patients, managing symptoms, and adjusting care plans.
– Consulting with patients managing chronic illnesses like cancer or HIV/AIDS.
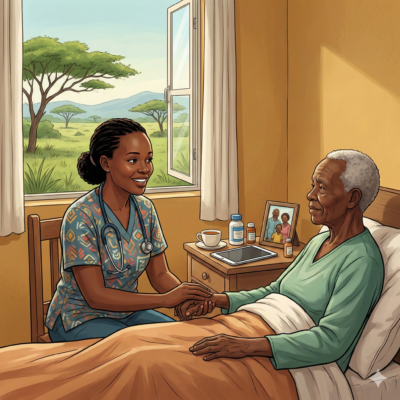
– Providing care to patients in their homes or in care homes.
– Collaborating with healthcare professionals to discuss patient care strategies.
What else might they be expected to do?
– Supporting both patients and their families throughout the illness trajectory.
– Facilitating discussions about treatment goals and advance care planning
– Addressing practical needs and providing bereavement counseling
– Training medical students, residents, or community health workers in palliative care principles.
What type of training is needed for this career path?
-Successful completion of Bachelor of Medicine and Bachelor of Surgery plus one-year internship in recognised institutions.
– Master of Palliative Medicine/ MSc. Palliative Medicine (3yrs) plus 2 years supervised practice.
– Registration with the Kenya Medical Practitioners and Dentists Council (KMPDC) or relevant regulatory bodies.
– Social workers, pharmacists, and other healthcare professionals may also work in palliative care, requiring relevant qualifications and registration.
What kind of personality is needed to excel in this career path?
– Empathy and Compassion: Essential for providing patient-centered care.
– Emotional Resilience: Ability to cope with end-of-life situations and patient suffering.
– Strong Communication Skills: Facilitating difficult conversations with patients and families.
– Team Collaboration: Working effectively within multidisciplinary teams.
What kind of interests do people in this career path have?
– Providing support and care to patients and their families (Helping)
– Treating complex medical conditions and developing care plans (Thinking)
Holland Codes: Helping (S) and Thinking (I).
Are there any innate skills or aptitudes required?
– High emotional intelligence and interpersonal communication.
– Understanding and respecting diverse cultural beliefs and practices.
– Problem-Solving Abilities
– Adaptability
What challenges can I expect to face if I pursue this career path?
– Emotional Strain: Regular exposure to terminal illness and death can lead to burnout.
– Resource Limitations: Especially in rural areas, there may be a lack of medications or trained personnel.
– Misconceptions about palliative care can hinder its acceptance and integration.
– Limited government support may affect program sustainability.
What are the job prospects for this path in Kenya and Africa? What about International prospects for a Kenyan citizen?
– Kenya and Africa: With the rise of chronic illnesses, there’s an increasing need for palliative care services. Kenya’s Ministry of Health released its first palliative care policy in 2021, aiming to integrate services nationwide.
– International: Countries with aging populations and advanced healthcare systems seek trained palliative care professionals.
What should I focus on if I choose to pursue this career?
– Cross-cultural communication and understanding of death and diseases
– Acquiring the prerequisite academic qualifications for practice
– Understanding your purpose. There is a high risk of depression and emotional burnout. Knowing why you chose this path can help you during hard times.
Related careers or job roles
– Palliative Care Psychiatrist
– Pain Management Specialist
– Hospice Medical Director
– Palliative Care Nurse
– Palliative Clinical Officer
– Palliative Social Worker
– Palliative Care Counselor or Psychologist